Individuals with private health coverage in the United States who seek emergency care from in-network hospital emergency departments (EDs) are often treated by out-of-network (OON) emergency physicians. A new UnitedHealth Group report reveals that inflated charges by OON emergency physicians treating patients at in-network EDs total an estimated $6 billion each year. The balance bills that often result from these charges are a key reason tens of millions of privately insured individuals struggle with high out-of-pocket costs.
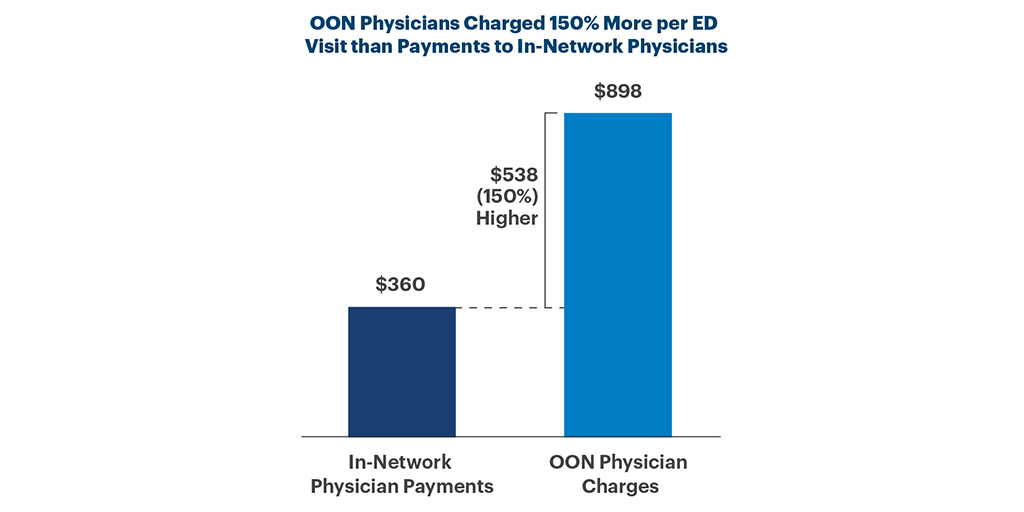
The report goes on to find that OON emergency physicians charged an average of 150 percent more per ED visit than in-network physicians were paid. The greatest total inflated charges by OON physicians during in-network ED visits were for the following health conditions:
- $1.9 billion in inflated charges for abdominal pain: 138 percent more per ED visit ($1,044 vs. $439)
- $1.6 billion in inflated charges for breathing problems: 158 percent more per ED visit ($841 vs. $326)
- $1.0 billion in inflated charges for chest pain: 136 percent more per ED visit ($1,155 vs. $490)
- $800 million in inflated charges for cuts, scrapes, and bruises: 153 percent more per ED visit ($754 vs. $298)
When health insurance plans pay higher prices for services delivered by OON providers, the increased costs put upward pressure on premiums and cost-sharing.
Share This Story